
Also in this section:
It is their responsibility to provide information and advice to their patients and their partners.
It is essential that the advice provided by healthcare professionals is up to date, consistent and evidence-based, in addition to the advice provided on other lifestyle choices such as drugs, smoking and nutrition.
Whilst this section follows DHSC usage and refers to pregnant women, this information applies to all pregnant people and National FASD fully supports non-discriminatory healthcare for all.
Guidance from the UK Chief Medical Officers regarding alcohol and pregnancy states:
“If you are pregnant or planning a pregnancy, the safest approach is not to drink alcohol at all, to keep risks to your baby to a minimum. Drinking in pregnancy can lead to long-term harm to the baby, with the more you drink the greater the risk.”
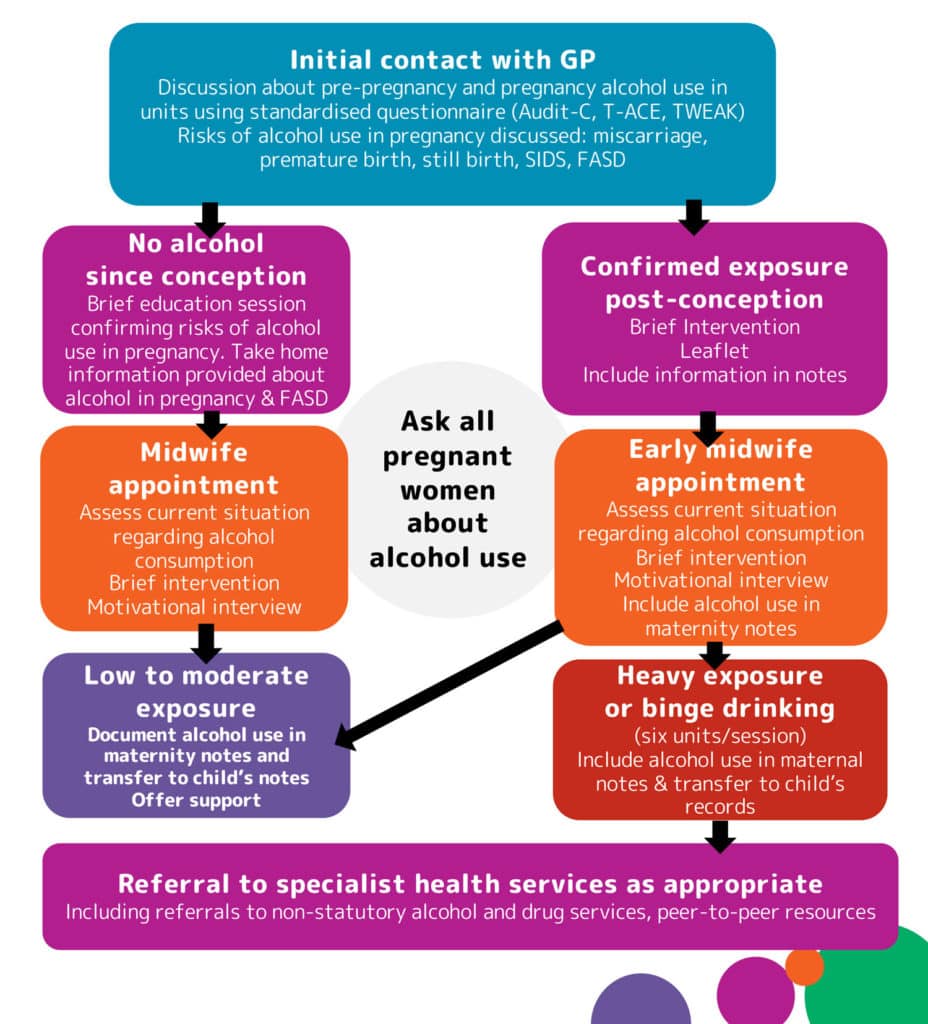
When you suspect a pregnant woman might be drinking alcohol, early intervention is the most effective way of improving the outcome for both mother and baby. An empathetic, non-judgemental approach encourages a positive response. No matter whether a woman is newly pregnant or nearly full-term, her baby will always benefit when she stops drinking (it is critical for in cases where alcohol withdrawal might be an issue that this is done with supervision). It is also important for mothers-to-be to have the support of the father, close family members and friends. When everyone is informed about the risks, better support can be in place for pregnant women.
It is believed that the fetus is affected by alcohol in two ways.
Other adverse outcomes of maternal alcohol consumption include:

Our new Midwives Toolkit is now available (including a free e-course).
Please feel to subscribe to our mailing list at the bottom of the page to stay up-to-date!
PHE’s latest document on alcohol in pregnancy
This includes statements on talking with pregnant women about alcohol and identifying alcohol-exposed pregnancies.
September 2021 journal article by Danijela Dozet, Larry Burd & Svetlana Popova in the International Journal of Mental Health and Addiction
Our midwives’ booklet (this will be updated soon)
Children and young people exposed prenatally to alcohol
(2016)
Greater Manchester Health and Social Care Partnership has an extensive project focused on alcohol-exposed pregnancies
Blackpool’s Better Start Programme
The National Organisation for FASD, The Priory, High Street
Ware, Hertfordshire. SG12 9AL
England
Helpline: 0208 458 5951