While FASD is primarily brain-based, it’s linked with a wide and sometimes overwhelming range of other conditions.
As a result, the lives of people with FASD can become very medicalised. This takes a toll on the individual and those who support them.
Healthcare professionals are not always aware of how challenging it can be to get a loved one out the door to these appointments.
Top tips:
There is so much more that can be said. This is just a start of the discussion, but National FASD felt it important to acknowledge how stressful this can be. Too often the team around those with FASD do not see the big picture of how hard it is to cope with these many appointments and conditions, all while looking after a loved one who has trouble processing what is happening, who struggles with transitions and different sights, smells, experiences and who has good reason to be wary of medical settings.
It is after all the bigger picture that affects our lives most.
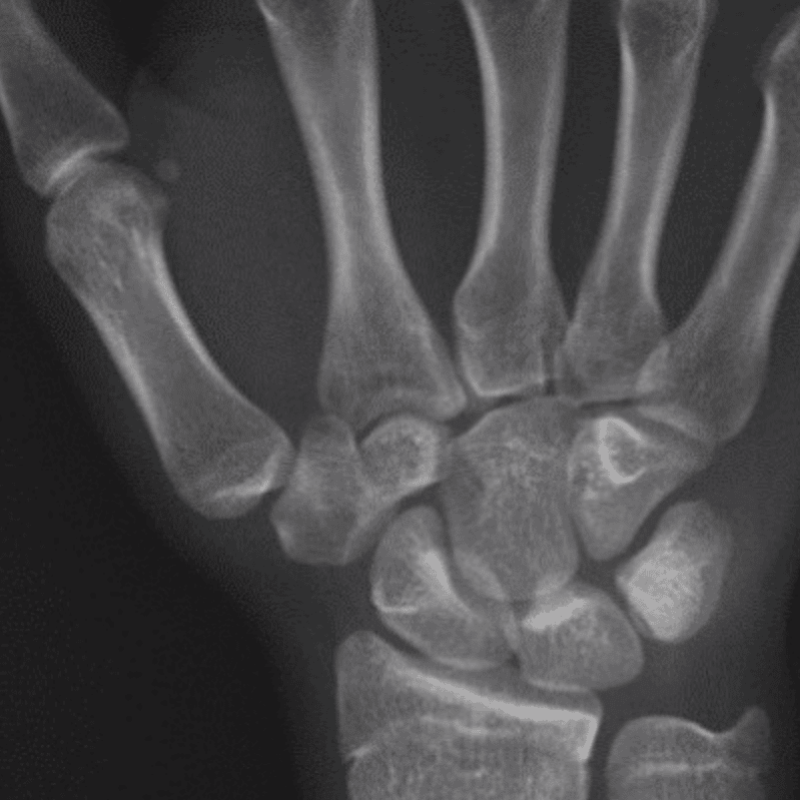
“There are not many days when we dwell in that place. Maybe you know it: the place where we are forced to imagine our loved one floating in the womb when the alcohol pulsed through his developing system. The place where we are forced to think very concretely about what parts of his body were damaged and when…
He is more tolerant of these appointments now. … In fact, he’s a little too comfortable in the setting, I thought, as I watched him skipping ahead of us, dancing and twirling down a long hospital corridor. I felt sad, a weight in my stomach. This child so full of life has spent too much time in too many hospitals… More medical appointments are being scheduled. It seems never-ending. Because it is. This is – and will be – his life.
I AM thankful, but simultaneously I tried to swallow down that internal scream I felt rising. What happened to this poor child? I just wanted to shout it. How is it possible so much of his system was so affected even before he first took a breath? Look! People, look! Don’t you see? The damage done is brutal…
We had envisioned a quick visit but had been in the hospital now for hours and hours. The waiting room had one obnoxiously loud toy that spat out balls that kept flinging everywhere and a train table with wooden tracks that did not fit in the space. This manic, frustrating play was a perfect storm brewing, even as my inner disquiet was growing.
I had finally been quite direct with them, saying our son has a disability, his meds would soon wear off, and was there any way to help us get out of there as soon as possible. We knew would be a very difficult car ride home, and it was. It’s now developed in his head that after a particularly intensive hospital visit he deserves a “treat.” So we stopped in a shop despite the risks that involved for overstimulation. Thankfully we found some scented play dough-type stuff. He smelled that and squeezed it during the car ride. We made it home okay-ish…
No one does this on purpose to a child. But prenatal exposure to alcohol has hurt our child deeply. It has quite literally affected him to his very core. And he is one of the luckier ones. It didn’t do its worst damage to him. Yes, I suppress the scream. Then I rally.
The National Organisation for FASD, The Priory, High Street
Ware, Hertfordshire. SG12 9AL
England
Helpline: 0208 458 5951